Doctor, are you listening? When doctors dismiss your symptoms
We’d made it about 200 meters from home when my mum cried out that she couldn’t walk another step. She slumped against someone’s front wall as I, a 14 year old girl, decided the best course of action.
My mum had a during my teenage years, but her symptoms were dismissed by most doctors. She would come back from the frustrated and feeling unheard.
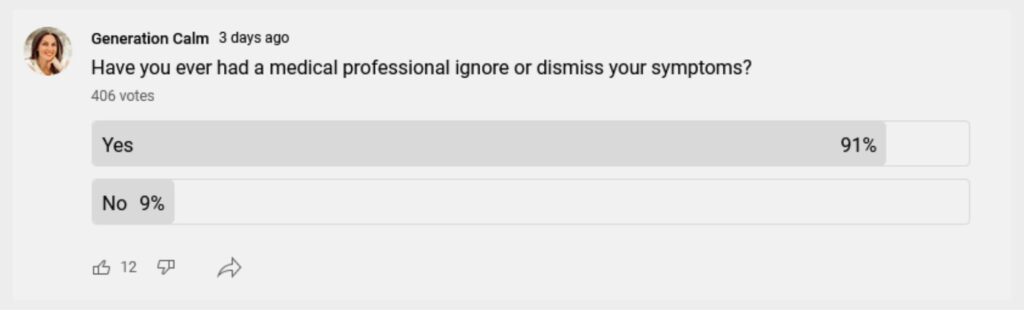
I was at home with mum every day, seeing her , frustration and very real of fatigue, headaches and nausea which would keep her mostly housebound. But the doctors dismissed her symptoms as being ‘all in her head’ or simply anxiety. Those doctors were doing what we would now call ‘‘.
She was eventually taken seriously by one who diagnosed her with M.E. (myalgic encephalomyelitis), a post-viral syndrome very similar to the Long-Covid we see today. Thirty years later, M.E. still has no treatment. But being able to put a label on a group of symptoms, and being taken seriously was so important for my mum’s healing. We’re lucky that my mum has long recovered from the illness. But for thousands of children and adults, this is an ongoing struggle.
Even the existence of M.E. (you’ve most likely heard it referred to as ) was refuted by many doctors, with newspapers giving it the nickname ‘yuppie flu’. For the last 30 years, patients have had their symptoms brushed off as psychosomatic. A cynical person might say it hasn’t had as much coverage from researchers and doctors because 75% of ME sufferers are women. Yes, gender bias still happens in the healthcare system!
What does m?
When a is questioning your account in a doubting way, not a curious way, this is called . Having your experience of symptoms be repeatedly challenged by a person of power, the doctor, is a manipulative form of communication.
Possible brush-off’s include:
- You are too young and healthy to be screened for that disease
- It’s to be expected ‘at your age’
- It’s your hormones
If you’ve had this experience before, you might find yourself saying, “I hope the will believe me”, before an appointment.
So how can you know if your is dismissing your very real as anxiety, a ‘‘s problem’ or as being ‘all in your head’?
How can you tell if your symptoms are psychosomatic or part of a physical illness? Remember, psychosomatic means that a psychological issue is causing … not that you’re making it up.
Is your mind or body causing your symptoms?
It can be difficult to tease out whether your are being caused by a mental health issue, like anxiety or something physical, like diabetes. But every knows to rule out biological reasons first, before assuming a mental reason.
The biopsychosocial model of care goes even further by looking at biological reasons, psychological reasons and social reasons for symptoms. An appointment with a is too short to cover all the bases which is why being self-aware is very useful. And this is why preparing before any appointment in the healthcare system is vital.
Here are some suggestions that can you do to prepare for a ‘s appointment to improve the chance that they’ll take your symptoms seriously.
Keep track of symptoms
You know your body better than anyone else, including a . So, when you feel off, you just know it. But unless you track when the symptoms occur, it can be difficult to explain the frequency, duration and severity of the symptoms to someone else.
Keeping an accurate record means using a calendar or chart to keep note of when a particular occurs. For my Mum’s M.E. this could have been to show when she was too fatigued to make dinner, had nausea, a headache etc. I have frequent headaches, so I use this printable headache diary.Here is another link to a printable pain diary.
Last year, I took a scribbled note of my inconsistent periods to my doctors appointments, just to read from. But both my GP and gynecologist took copies of these dates I’d hastily scribbled down. They’re invaluable because they’re real data points. Doctors can use these numbers. Rather than telling them I have inconsistent periods, they now have a more accurate picture. They can use this to form a more accurate diagnosis.
And tracking is also empowering for you. By tracking medication, monitoring the frequency, duration and severity of your symptoms over time, you can more easily identify patterns which may provide clues to a trigger. All of this extra information puts you in control.
Tracking your symptoms can come in all shapes and varieties from pretty trackers in bullet journals to apps for specific health conditions. Find one that makes it easy for you to track.
![]()
Use helpful words to describe the pains or sensations
Often, it’s hard to put a finger on symptoms and how they feel. Especially some ethereal symptom, like brain fog. When talking to a doctor, you are not trying to analyze the symptoms, but merely describe what it’s like. You don’t need to know medical terminology to describe your symptoms.
For example, when trying to describe a pain some of the following words could be helpful:
- burning sensation
- throbbing
- stabbing
- gnawing
- squeezing
- a feeling of pressure
- feels hot
- achey
Followed by how often:
- intermittent
- constant
- worse when I’m moving
- worse when stationary
- worse when I touch it
- so often I’ve give up many activities
Ending with how intense:
- so painful I can’t concentrate
- I can continue with my usual routine … just more slowly
- my pain is hardly noticeable
- it stops me from sleeping
And explain how the symptoms have affected your day to day life. This is powerful. Instead of saying ‘I need to urinate a lot’, say ‘I have to interrupt my work mid-meeting to go to the bathroom’. This shows how it impacts your life and those around you.
Shop around
When doctors dismiss your symptoms, please go to a different medical provider until you find one that acts like they are genuinely interested. Doctors are real people. There could be a variety of reasons why they’re not paying enough attention to you – a workload that surpasses what a human can take on, burnout, a family bereavement, a personal life in turmoil – but you need someone who will take you seriously.
Yes, there are some crappy doctors. But, in reality, most doctors want to help you.
Having a list of symptoms and dates or charts will help them tease out whether the symptoms are physical or mental. But if that doesn’t work, move on.
Mindset matters
You have a set of beliefs about doctors, clinics and illnesses. This set of beliefs has been molded from a young age by those around you, the way loved ones talk about illness and your personal experiences with the medical system. When you enter a medical facility, these beliefs come with you. Whether you acknowledge it or not, your prejudices and stereotypes will follow you into the doctor’s office.
You won’t be able to drop your beliefs outside the clinic door, but it will be helpful to have a mindset of openness before your appointment. Notice if you are feeling apprehensive, frustrated or mistrustful. See if you can leave that behind you and go into the appointment knowing that you (and your doctor) are both doing the best you can. This will help you feel calmer so you can politely continue a conversation with a in a confident and assertive manner.
I know you’ve probably Googled your symptoms already, perhaps even come up with your own diagnosis. But doctors see people all day long, they get a good overview of clusters of symptoms much more than a medical website. Be open to their ideas.
Communication skills
Even if you are the best communicator in the world, when you are a patient these skills may be limited. Pain, depression and anxiety can all prevent a person from communicating effectively.
In a doctor-patient relationship there is an uneven power at play. The doctor holds the cards. If you find it intimidating to go to a , have communication difficulties or believe that your doctor may harbor prejudices that impacts their judgement, arrange to bring a trusted friend, spouse, or parent along to the appointment. Even if your companion doesn’t talk, it can help you feel more calm. And the doctor may be more communicative if there are two people in the room.
If this is not possible, contact a patient advocate service, they can help you get your point across.
But you can be in control of improving your communication skills. While waiting for your doctor to arrive, spend a few quiet moments thinking about what points you want to get across. If you could boil it down to one main message, what would it be? Instead of flipping through a magazine or scrolling your phone, use this valuable time to get clear on your thoughts, it will lead to better communication.
And keep a running list of questions so you remember to ask about specific matters. Asking questions can illicit topics that might not have come up otherwise because the clinician didn’t feel it was relevant.
Regardless of how dismissive your doctor is, it’s very important to stay calm, positive and not be passive aggressive. If your doctor is consistently dismissive, politely leave then find another clinician.
Set an intention before your appointment
While you don’t want to tell your doctor what to do, it is possible to help increase the chances of things going well, by setting an intention for your appointment. Writing down what outcome you would like helps you to hone your message. So what’s the best-case scenario you’d like from this appointment? Know beforehand so that you can steer the conversation there. Examples might be, to get a referral to a specialist; to get tested for a specific deficiency; or to be prescribed a medicine.
Conclusion
I know this sounds like you’re putting in a lot of work beforehand, but planning ahead helps you feel prepared, less flustered and more confident. The onus should not have to all be on you, but some doctors have very little training in patient communication skills, depending on when and where they were trained. So if you do your very best to communicate and they still fall short, it’s time to find another doctor.
Some chronic illnesses, even though they have a physical cause, may not show up with testing. Things like , long COVID and . So settle in for a long process of ruling out other illnesses. It’s normal, it doesn’t mean your doctor doesn’t believe you.
Don’t let one bad clinician put you off going to an appointment. You should always see a for any new or lingering symptoms. Please don’t let a previous encounter with a put you off seeking .
If you like this blog post, you’ll enjoy being part of my fortnightly newsletter. You can sign up to the right, to the right ➡➡

